Infection Prevention Policy
Our infection prevention and control policy covers the following:
Section 1: General Infection Prevention & Control
Section 2: Responsibilities for Infection Control
Section 3: Cleaning
Section 4: Blood & Body Fluid Spillage
Section 5: Disposal of Clinical Waste
Section 6: Safe Use & Disposal of Sharps
Section 7: Needle stick
Section 8: Hand Hygiene
Section 9: Using Personal Protective Equipment
Section 10: Natural Rubber Latex
Section 11: Specimens for Clinical Laboratories
Section 12: Management of Infectious Diseases
Section 13: Protection from Hepatitis B
Section 14: Varicella Zoster (Chicken Pox)
Section 15: Treatment of MRSA Catheter Urine
Section 16: Treatment of MRSA Positive Wounds
Section 17: Rubella
Section 18: Minor Surgery
Section 1 – General Infection Prevention and Control
Patients receiving health and social care are at risk of developing infection as a result of their compromised state of health, underlying medical conditions, or as a result of contact with health care interventions such as surgery, diagnostic testing or invasive devices.
In addition, health and social care settings can provide ideal conditions for micro-organisms to be transmitted between those who receive and give care. The close proximity and contact between each party and the continuous contact in a shared working and living environment all contribute to transmission.
The Practice has an Infection Control Lead to whom any concerns should be reported.
The Essential Principals of Infection Prevention & Control are:
1. Hand Hygiene.
2. Using Personal Protective Equipment.
3. Safe Handling and Disposal of Sharps.
4. Safe Handling and Disposal of Waste.
5. Spillage Management.
Section 2 – Roles and Responsibilities for Infection Prevention and Control
The Infection Prevention and Control Lead
The Lead will:
- Act as an infection prevention and control champion.
- Promote good practice and provide advice and support to colleagues within the workplace, acting as an advocate for patients, families and carers.
- In liaison with other relevant staff preparing, reviewing and updating evidence based policies and guidelines in line with relevant Department of Health notifications and/or national guidelines, when available and applicable.
- Distribute policies to relevant areas and initiate their implementation by means of support, advice and education.
- Ensure that compliance with Infection Prevention and Control policies are monitored as appropriate.
- Attend, contribute to and deliver identified training sessions, and pass attendance records for updating employee training records.
- Disseminate pertinent information within the workplace in an appropriate and timely manner.
- Undertake audits of infection control procedures and cleanliness.
- Inform the Partners and Operations Team of any serious problems or issues relating to Infection Prevention and Control.
- Ensure liaison with the Human Resources Department and Occupational Health Department with regard to staff health and transmission of infectious disease.
Role of Individual Staff Members
- All employees will be personally accountable for their action and are responsible for ensuring that they comply with Infection Prevention and Control policies.
- Employees must understand their legal duty to take reasonable care of their health, safety and security and that of other persons who may be affected by their actions and for reporting untoward incidents and areas of concern.
- Healthcare workers are responsible for identifying infectious conditions and circumstances that may lead to outbreaks of infection that require specific controls to protect themselves, their patients or others.
- They are responsible for notifying the Infection Prevention and Control Lead of such circumstances and it is the responsibility of healthcare workers to ensure that they utilise safe working practices as outlined in Infection Prevention and Control policies.
- Any breach in Infection Prevention and Control Policies or Practice will place staff, patients and visitors at risk and subsequently the completion of a significant event form will be required.
Responsibilities to the Public
One of the key aims of this policy is the promise to maintain a clean and safe environment which includes having staff who understand the need for effective hand hygiene throughout their working day.
Other responsibilities to the public include:
- Provision of appropriate patient information leaflets regarding alert organisms.
- Disseminating information regarding any measures to control the spread of infection, including outbreaks, by appropriate signage at key entry points to the Practice and individual clinical areas or by verbal guidance from staff.
- Promoting a culture which encourages the public to challenge staff who are failing to wash their hands.
- The Practice requests that the public also play their role in minimising the risk of infection by helping to keep the Practice environment clean.
Section 3 – Cleaning
Denton Medical Practice work closely with the cleaning company they have contracted for cleaning.
These specifications have four main aims:
- to assist in ensuring the infection risks posed by the delivery of services has been assessed.
- to provide a framework through which cleaning services can be arranged to address those risks.
- to ensure that appropriate documentation is available to show how the above processes have been managed and implemented.
- to emphasize that cleaning is a shared responsibility involving more than the cleaning team.
Audit and inspection policies are also required to ensure cleaning services are regularly monitored, any shortcomings identified, remedial actions taken, and that there is a clear and robust audit trail in place.
Section 4 – Blood and Body Fluid Spillage
Spillage of blood and body fluids must be dealt with quickly and effectively. Disposable gloves and apron must be worn and contaminated debris treated as clinical waste. Chlorine-releasing agents can be a hazard especially if used in large volumes, in confined spaces or mixed with other chemicals or urine.
Protective clothing must be worn and the area well ventilated. A risk assessment and COSHH assessment must be carried out if using these chemicals. Increased risk is related to the likelihood of infection.
Section 5 – Disposal Of Clinical Waste
What is Clinical Waste?
Clinical Waste is something which unless rendered safe may prove hazardous to any person coming into contact with and include:
- Human or animal tissue.
- Blood or bodily fluids.
- Excretions.
- Drugs or other pharmaceutical products.
- Swabs or dressings.
- Syringes, needles or other sharp instruments.
These hazardous wastes are managed carefully within our surgeries and are managed by our cleaning company in conjunction with our clinical staff.
Section 6 – Safe Use and Disposal of Sharps
The aim of this policy is to ensure that sharps are used and disposed of safely within Denton Medical Practice.
This policy applies to all employees of Denton Medical Practice to manage contamination and sharps related incidents correctly and safely.
For the purpose of this policy a ‘sharp’ is defined as anything which may puncture the skin and which may be contaminated by blood or other bodily fluids. The vast majority of sharps injuries are avoidable, and occur when sharps are handled or disposed of in an unsafe manner. Staff must follow this guidance in order to minimise the likelihood of sharps injuries occurring.
The surgeries are equipped with containers to receive used sharps; these are carefully dated, sealed and disposed of in an appropriate fashion.
Audits are undertaken regularly to ensure the policy is complied.
Section 7 – Needle Stick
Needle stick injuries are a day to day hazard of performing injections and procedures on patients.
The practice has a detailed policy as to how to manage needle stick accidents, which potentially put our staff at risk of serious infection.
All such incidents are taken very seriously and appropriate treatment given.
Patients may be asked to give blood samples if they are involved in an incident involving an injury to a member of staff.
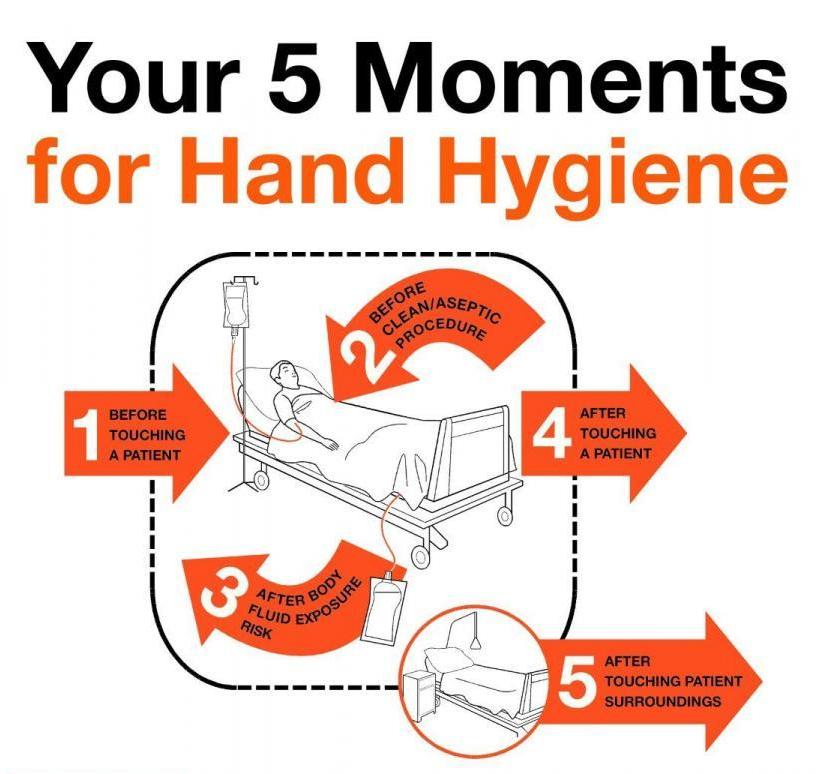
Section 8 – Hand Hygiene
It is well known that hand hygiene is one of the most important factors in preventing the spread of infection and the unwashed hands of all healthcare professionals is the most important route of cross-infection in the healthcare environment. It is therefore vitally important that healthcare organisations have a robust hand hygiene policy in place in order to minimise the risk of cross infection via the hands of their healthcare workers.
Every member of Denton Medical Practice staff will understand the importance of hand hygiene and will be able to practice good hand decontamination at the appropriate time.
Section 9 – Using Personal Protective Equipment (PPE)
Personal protective equipment (PPE) is used to protect both health care workers and patients from risks of infection. The risk of infection occurring is reduced by preventing the transmission of micro-organisms to the patient via the hands of staff or vice versa. Gloves may also be required for contact with hazardous chemicals and some pharmaceuticals, for example, disinfectants or cytotoxic drugs. PPE includes items such as gloves, aprons, masks, goggles or visors.
Please see below the related policy for Natural Rubber Latex for use of gloves.
Section 10 – Natural Rubber Latex
This policy has been written to provide guidance for health care professionals using natural rubber latex (NRL) gloves. It is based on the Health Safety Executive information on the use of natural rubber latex gloves.
Reactions to NRL gloves and other products impact on GPs and nurses because:
- They are at increased risk of developing NRL allergy through the repeated use of wearing NRL gloves.
- It is possible healthcare professionals may need to manage NRL-sensitive patients. These patients may be known to them in advance or previously undiagnosed.
- Healthcare professionals have a statutory responsibility to reduce risk of sensitisation in themselves, their colleagues and patients.
- It is recognised that GPs and practice nurses are frequently the first port of call for sensitised patients who may or may not suspect that they have an NRL allergy. It is important that GPs are able to identify patients with suspected NRL allergy to allow prompt referral to a diagnosing physician (dermatologist or immunologist) for further investigation.
Section 11 – Specimens for Clinical Laboratories
- Ensure all specimens are labelled correctly.
- The freshness of the specimen determines its usefulness, so get all specimens to the laboratory as soon as possible.
- All specimens are potentially dangerous so should be bagged and must be transferred to laboratories in proper rigid containers.
- Contaminated, leaking and unlabelled specimens will be discarded. Urines samples must be disposed of in waste facility in dirty utility rooms & sample bottled placed in clinical waste bins, blood bottles should be placed in sharps bins.
- Label specimens ‘HIGH RISK’ when appropriate.
- Ensure that legible clinical details are including antibiotics taken on all microbiology specimens.
Section 12 – Management of Infectious Diseases
Infectious diseases are caused by pathogenic microorganisms, such as bacteria, viruses, parasites or fungi; the diseases can be spread, directly or indirectly, from one person to another. Zoonotic diseases are infectious diseases of animals that can cause disease when transmitted to humans.
If a member of staff contracts an infectious disease, they should notify the management team and the HR department - see link: Infectious Diseases A to Z
The Management Team and HR will review each case individually and decide on a management plan which will review whether a member of staff is fit to work and if so in what capacity.
Section 13 – Protecting Staff and Patients from Hepatitis B
The Practice will:
- Make arrangements to ensure that all staff are offered immunisation against Hepatitis B.
- Ensure staff are given information and guidance on the risks of contracting Hepatitis in respect of their work/training.
- Implement procedures for dealing with staff that become infected with Hepatitis B or are carriers of the virus.
- All staff are expected to co-operate in arrangements made for protecting them against risk and to comply fully with the provisions of these guidelines.
Section 14 – Varicella Zoster (Chicken Pox)
Varicella zoster is a highly infectious disease and can be reactivated in the form of Herpes Zoster (Shingles). It is spread by direct physical contact with an infected person or by droplet infection.
All staff in clinical contact with patients should be tested for varicella zoster antibodies unless they are definite that they are varicella zoster immune following a prior antibody assessment. The result should be documented in their personal file.
The Practice will:
- Make arrangements to ensure that all members of the Practice Team, who may be required to become in clinical contact with pregnant women, are screened and, where they are found not to be immune will be offered immunisation against chicken pox.
- Ensure that members of the Practice Team are given information and guidance on what action to take if they have been in contact with chicken pox in respect of their work.
- Implement procedures for dealing with staff that become infected with chicken pox.
- Female Staff will be asked to avoid pregnancy for three months after receiving the vaccine and asked to sign a consent form for receiving a varicella zoster vaccine.
All staff are expected to co-operate in arrangements made for protecting them against risk and to comply fully with the provisions of these guidelines.
Sections 15 & 16 – Treatment of Catheter Urine MRSA Positive Results and Wounds
Important Notes on MRSA Decolonisation
- All treatment should be used when decolonising regardless of where patient is positive the body wash and nasal ointment should be used.
- In the event that any remain, all unused treatments should be disposed.
- 48 hours after treatment has discontinued (72 hours if the course finishes on a Friday) rescreen all sites – swab nose, groin, any wounds (identify each swab with wound site), sputum if patient is expectorating, CSU if catheterised.
- If all specimens are negative for MRSA then re-screen at weekly intervals until 3 negative results obtained. * If any specimen is positive, recommence decolonisation regime.
- Urine – if remains positive discuss with Consultant Microbiologist.
- Wounds – Mupirocin is not to be applied directly to wounds only nasal use. Recommend silver/medihoney/iodine based dressings.
- Antibiotic Advice – Please contact the Consultant Microbiologist or the Infection Prevention and Control Team if systemic antibiotics are considered.
Section 17 – Rubella
Measles is an acute viral illness caused by a morbillivirus of the paramyxovirus. Measles is spread by airborne or droplet transmission. Incubation period is about 10 days (ranging between 7 and 18 days) with a further 2 to 4 days before the rash appears.
Mumps is an acute viral illness caused by a paramyxovirus. Mumps is spread by airborne or droplet transmission. Incubation period is around 17 days (ranging between 14 to 25 days). Individuals with mumps are infectious from several days before the parotid swelling to several days after it appears.
Rubella is a mild disease caused by a togavirus. Rubella is spread by droplet transmission. Incubation period is 14 to 21 days, (with majority of individuals developing a rash 14 to 17 days after exposure). Individuals with rubella are infectious from one week before symptoms appear to 4 days after onset of rash. Maternal infection within the first 8 to 10 weeks of pregnancy results in damage in up to 90% of infants, the risks declines to about 10% to 20% between 11 to 16 weeks.
All staff in clinical contact with patients should be tested for measles and rubella antibodies unless they are definite that they are measles, rubella immune following a prior antibody assessment. The results should be documented in their personal file.
Section 18 – Minor Surgery
This Policy, in conjunction with national guidance documents, relates to the prevention and control of infection at Denton Medical Practice through effective cleaning systems.
Denton Medical Practice work closely with the cleaning company they have contracted to clean the minor surgery room.